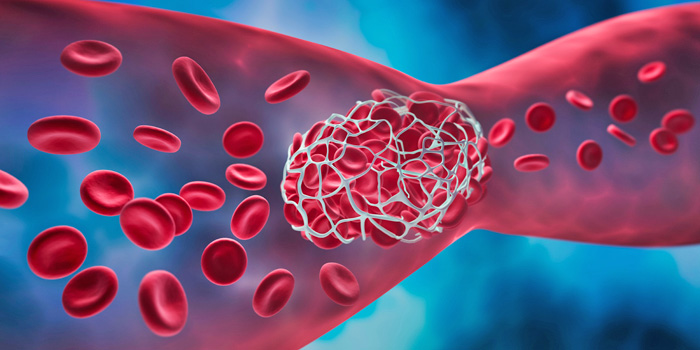
Today, many seniors take anticoagulants which keep blood “thin” thus preventing clots that may lead to coronary artery disease, deep vein thrombosis, a stroke or a heart attack or complications following some surgeries. In reality, anti-coagulants do not actually make blood ‘thinner’ but create an environment in which blood clots have more difficulty forming.
Elderly patients represent a population at high thromboembolic (blood clot) risk, but also at high hemorrhagic (excessive bleeding) risk. Therefore, assessing the benefit-risk ratio of anticoagulation is one of the most challenging issues in the management of these patients.
Types of Blood Thinners
There are two main types of blood thinners: Warfarin and direct oral anticoagulants (DOACs). Warfarin is an older drug that has been used for decades. It works by interfering with the production of vitamin K which is needed for blood clotting. Warfarin requires regular blood tests to monitor the level of anticoagulation and adjust the dose accordingly. It also interacts with many foods and drugs that can affect its effectiveness or safety.
DOACs are newer drugs that have been introduced in the past decade. They work by directly blocking specific enzymes or factors involved in blood clotting. DOACs do not require blood tests or dose adjustments and have fewer interactions with foods and drugs. However, they are more expensive than Warfarin and may not be covered by some insurance plans. They also have no antidote to reverse their effects in case of bleeding emergencies.
Side Effects
Possible side effects of blood thinners in the elderly include back pain, bowel or bladder dysfunction, easy bruising, blood in urine or feces, and black or dark-colored stools. More serious side effects can include uncontrollable bleeding and vomit that resembles coffee grounds.
Also, older adults are more likely to have other medical conditions, take other medications, and experience falls or injuries that can cause bleeding. Therefore, care must be taken when taking blood thinners.
Certain foods and medications can either increase or decrease the action of blood-thinning drugs, especially for the anticoagulant Warfarin. Patients should be aware of these potential interactions and adjust their diet or medication regimen accordingly under the guidance of a healthcare provider.
Precautions
Seniors who take blood thinners should follow some precautions to minimize the risk of bleeding and maximize the benefit of stroke prevention. These include:
- Taking the medication as prescribed and not missing or doubling doses.
- If taking Warfarin, having regular blood tests and following the doctor’s instructions on dose adjustments.
- Informing the doctor of any changes in diet, medication, or health status that may affect the blood thinner’s effectiveness or safety.
- Avoiding or limiting alcohol, which can increase the risk of bleeding and interfere with the blood thinner’s action.
- Avoiding or using caution with over-the-counter drugs, supplements, or herbal remedies that may interact with the blood thinner. These include nonsteroidal anti-inflammatory drugs, such as ibuprofen or naproxen, vitamin K supplements, green tea, or foods rich in vitamin K, such as leafy greens, broccoli, or liver, any of which can increase the risk of bleeding.
- Seeking medical attention immediately if experiencing any signs or symptoms of bleeding, such as bruising, nosebleeds, gum bleeding, blood in urine or stool, black or tarry stool, coughing up blood, vomiting blood, severe headache, dizziness, weakness, or fainting.
- Wearing a medical alert bracelet or carrying a card that identifies the type of blood thinner being used, in case of an emergency or injury.
- Consulting the doctor before undergoing any surgery, dental procedure, or invasive test that may require stopping or adjusting the blood thinner.
- Wearing gloves while doing yard work.
- Carefully using scissors or knives.
- Using an electric razor or hair removal cream instead of razor blades.
- Using waxed dental floss instead of toothpicks.
- Using a soft bristle toothbrush.
- Using caution when cutting finger and toenails.
Managing Bleeding
If bleeding occurs while on blood thinners, it’s recommended to press firmly against the bleeding part with a damp washcloth or tea bag for 30 minutes. If the bleeding does not stop after two hours, it’s important to contact a healthcare provider.
In Sum
While blood thinners can be beneficial for elderly individuals at risk of blood clots, it’s crucial to be aware of the potential side effects and to manage these risks through careful monitoring and adjustments to activity, diet, and medication regimens. Always consult with a healthcare provider for personalized advice and treatment plans.